A newly identified measles case in Victoria with no overseas travel history has health officials concerned about local transmission of the highly contagious disease. The case brings Victoria’s total to 15 measles infections this year, with five now confirmed as locally acquired.
Victoria’s Chief Health Officer has issued a public health alert as the infected person visited multiple locations across Melbourne and Gippsland while contagious, creating numerous exposure sites where others may have contracted the virus.
“There is an increased risk of measles in the greater Melbourne area, with a number of new exposure sites identified,” states the Department of Health advisory. “A growing number of measles cases have acquired their infection locally in Victoria.”
Health experts note this pattern marks a significant shift from the typical pattern where measles cases are usually linked to international travel.
The current situation reflects a broader national trend, with Australia reporting 59 measles cases so far in 2025, already surpassing the 57 cases recorded throughout all of 2024.
Exposure Sites Require Vigilance
Health authorities have published a detailed list of exposure sites spanning Melbourne and Gippsland, including shopping centers, restaurants, healthcare facilities, and public transport. Anyone who visited these locations during specified times should monitor for symptoms until 18 days after exposure.
Recent exposure sites include Westfield Fountain Gate in Narre Warren, St. Vincent’s Hospital Emergency Department in Fitzroy, multiple retail stores, restaurants such as Johnny, Vince and Sam’s Ristorante in Carlton, and various healthcare facilities.
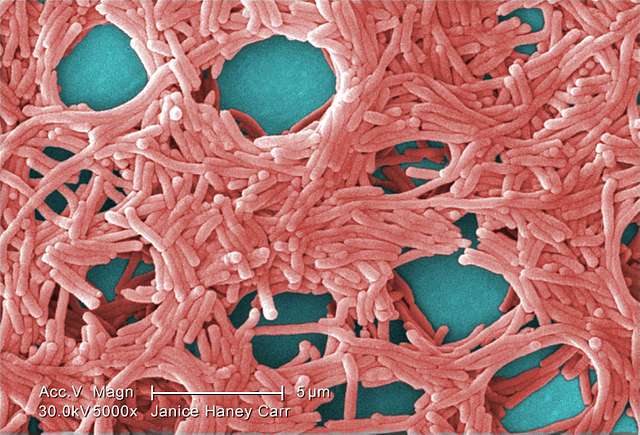
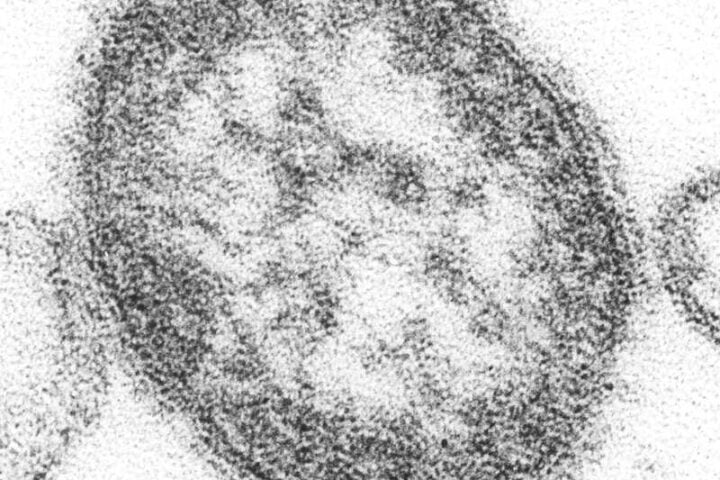
The measles virus is remarkably persistent, remaining active in the air or on surfaces for up to two hours after an infected person has left an area.
Similar Posts
Symptoms and Vulnerability
Measles typically appears 7-18 days after exposure, beginning with fever, runny nose, red eyes, and cough, followed by a distinctive rash that starts on the face and spreads downward. Small white spots inside the mouth, called Koplik’s spots, often appear before the rash and serve as a key diagnostic indicator.
Professor Margie Danchin from the Murdoch Children’s Research Institute expressed “huge concern” over recent outbreaks and declining vaccination rates since the COVID-19 pandemic.
Several groups face heightened risk:
- Unvaccinated individuals
- Infants under 12 months who cannot yet receive full vaccination
- People with weakened immune systems
- Adults born between 1966 and 1992 who may have received only one dose of the MMR vaccine
Prevention and Protection Measures
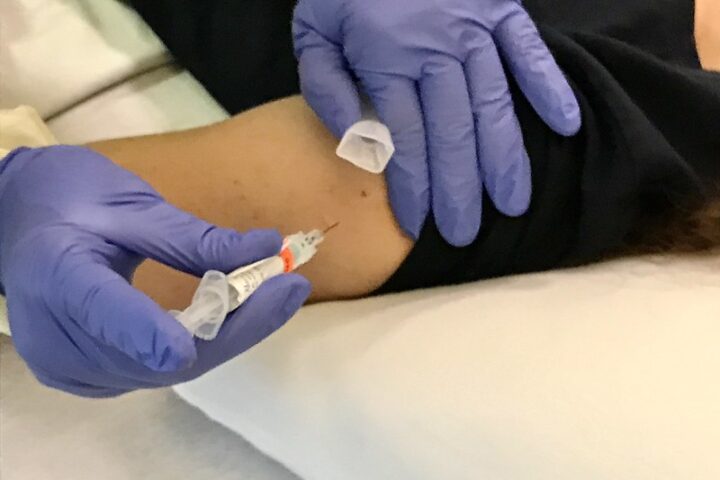
The MMR (measles-mumps-rubella) vaccine remains the most effective protection, with two doses providing approximately 97% immunity against measles.
Health authorities urge all Victorians born during or after 1966 to check their vaccination status and receive free catch-up vaccines if needed. The vaccine is available from GPs, pharmacies, local councils, and Aboriginal Health Services.
For those potentially exposed to measles:
- The MMR vaccine can prevent illness if given within 72 hours of exposure
- Normal human immunoglobulin (NHIG) may protect vulnerable individuals like infants and pregnant women if administered within six days of exposure
Anyone developing symptoms should seek medical attention immediately, wearing a mask and calling ahead to ensure proper isolation procedures.
“Anyone who develops symptoms of measles should seek medical care and testing,” advises the Department of Health. “Call the health service beforehand and wear a face mask.”
Healthcare Response
Medical professionals across Victoria have been asked to maintain heightened vigilance for possible measles cases, especially in patients without recent travel history.
The Royal Australian College of General Practitioners has provided resources to help doctors recognize, test for, and manage potential cases. Suspected cases should be immediately reported to the Department of Health and isolated under airborne precautions.
Dr. Tim Jones, Chair of RACGP Specific Interests Child and Young Person’s Health, noted “increasing concern” about the doubling of measles cases alongside falling vaccination rates.
Global measles outbreaks in regions including Vietnam, Thailand, India, Africa, Europe, the UK, the Middle East, and North America contribute to the risk of imported cases through international travel.
Chief Medical Officer Professor Anthony Lawler acknowledged the rising cases across Australia but advised that while Australians “should not be alarmed,” they should take appropriate precautions and verify their information sources regarding measles and vaccination.
The current situation underscores the critical importance of maintaining high vaccination coverage to protect both individuals and the broader community through herd immunity.
Frequently Asked Questions
Measles symptoms typically appear 7-18 days after exposure. Early symptoms include high fever (39-40°C), runny nose, red/sore eyes (conjunctivitis), and cough. Around day 2-3, small white spots (Koplik’s spots) may appear inside the mouth. A distinctive red, blotchy rash usually appears 3-5 days after initial symptoms, starting on the face around the hairline and spreading down to the neck, trunk, arms, and legs. If you develop these symptoms after possible exposure, seek medical attention immediately, wear a mask, and call ahead to notify the healthcare facility.
You may have been exposed if you visited any of the listed exposure sites during the times specified by health authorities. These include multiple locations across Melbourne and Gippsland, such as Westfield Fountain Gate in Narre Warren, St. Vincent’s Hospital Emergency Department in Fitzroy, restaurants like Johnny, Vince and Sam’s Ristorante in Carlton, and various other public places. The Department of Health maintains an updated list of exposure sites on their website. Anyone who spent time in greater Melbourne or Gippsland from mid-March should be alert for possible exposure and monitor for symptoms for up to 18 days after potential contact.
Measles is one of the most contagious infectious diseases known. It spreads through airborne droplets released when an infected person coughs or sneezes. These droplets can remain suspended in the air or settle on surfaces, where the virus can survive for up to two hours after the infected person has left the area. A person with measles is contagious from about 24 hours before showing initial symptoms until four days after the rash appears. One infected person can potentially infect 9 out of 10 unvaccinated people who come into contact with them, making it crucial to isolate suspected cases quickly.
You’re likely protected against measles if you’ve had two doses of the MMR (measles-mumps-rubella) vaccine, which provides about 97% immunity. People born before 1966 are generally considered immune due to widespread exposure to the virus. However, those born between 1966 and 1992 may have received only one dose, as the second dose wasn’t routinely recommended until later. To check your vaccination status, look at your immunization records, contact your GP or the Australian Immunisation Register. If you’re unsure or haven’t had two doses, you can receive a free catch-up MMR vaccine from your GP, pharmacy, local council, or Aboriginal Health Service. No blood test is needed before vaccination.
If you think you’ve been exposed to measles, monitor yourself for symptoms for 18 days after exposure. If you’re not fully vaccinated and were exposed within the last 72 hours (3 days), you may be eligible for the MMR vaccine as post-exposure prevention. Pregnant women, infants, and immunocompromised people who aren’t fully vaccinated should seek medical review within 6 days of exposure for possible preventive treatment. If you develop symptoms, call ahead to your healthcare provider before visiting, mention your possible measles exposure, and wear a face mask. Stay isolated from others to prevent potential spread until measles has been ruled out.
While measles can be serious for anyone, certain groups face higher risks of severe complications. These include unvaccinated infants under 12 months of age, pregnant women without immunity, people with weakened immune systems due to conditions or treatments, malnourished individuals, and those with vitamin A deficiency. Possible complications include ear infections, pneumonia, encephalitis (brain inflammation), and in rare cases, a fatal degenerative brain disorder called SSPE (Subacute Sclerosing Panencephalitis) that can occur years after infection. These vulnerable groups should be particularly vigilant about avoiding exposure and should seek immediate medical attention if exposure is suspected.