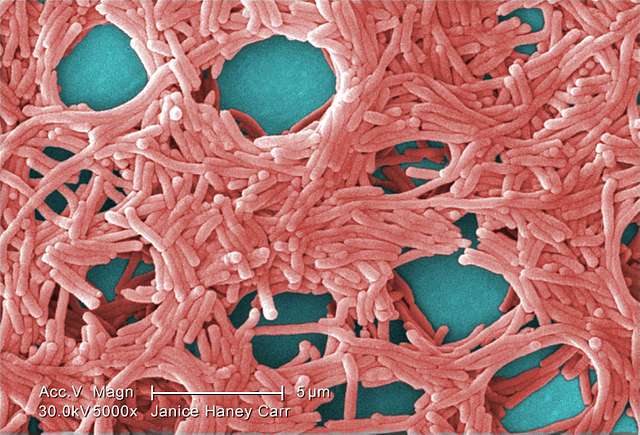
In a groundbreaking study by the University Medical Center Utrecht’s Center for Translational Immunology, researchers have unveiled critical insights into why some people suffer from chronic pain after an initial injury or inflammation. This research, led by Hanneke Willemen, PhD, and Niels Eijkelkamp, PhD, is a significant stride in the medical community’s understanding of pain management. The study highlights that inflammation, the body’s primary response to injury and pathogens, is a key driver of pain. Interestingly, the research also reveals that nicotinamide riboside, a form of vitamin B3, has been effective in alleviating persistent pain in mice. This finding suggests the potential for new treatments for chronic pain in humans, especially for those who continue to experience pain even after the initial inflammation has resolved.
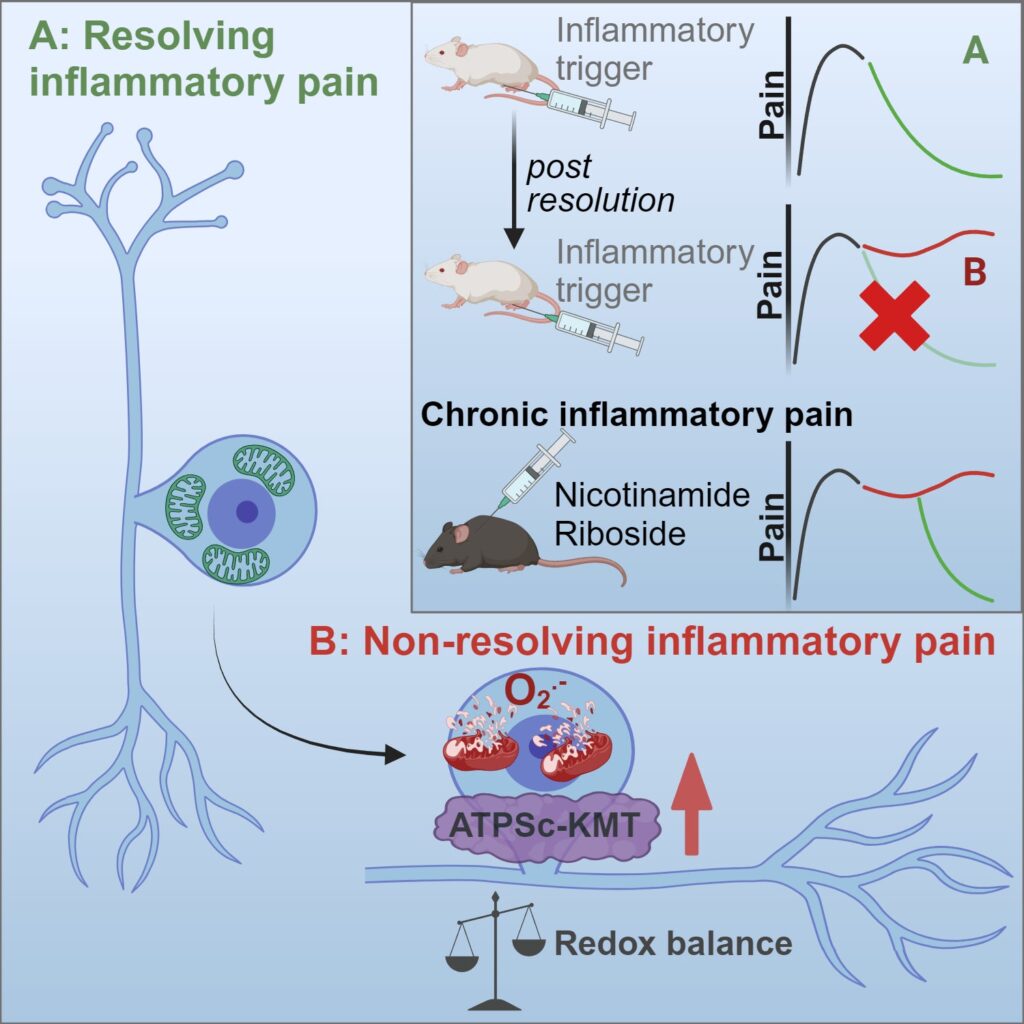
The crux of their findings revolves around a process known as hyperalgesic priming. Imagine this: you injure your foot, and it heals, but the pain lingers or even worsens over time. This phenomenon is what the study aimed to decode. The researchers discovered that the key lies in the sensory neurons – the nerve cells responsible for sending pain signals to our brain.
During their experiments with mice, the team observed that a short-term inflammation could lead to long-lasting changes in these neurons. Specifically, they noticed disturbances in mitochondria, the powerhouses of our cells, and redox processes, which involve the transfer of electrons in our body. These changes were linked to a protein called ATPSc-KMT, previously associated with chronic pain in patients.
Similar Posts
Here’s where it gets fascinating: by tweaking mitochondrial function and managing ATPSCKMT expression, the researchers could reverse the lingering pain in their animal models. This approach, along with supplementing certain metabolites, showed promise in preventing the shift from temporary to chronic pain.
“In our study we provide evidence that a peripheral inflammation induces persistent mitochondrial and metabolic changes in sensory neurons, which affects the ability of neurons to resolve from hyperalgesia induced by a subsequent inflammatory trigger. Thus, metabolic changes in sensory neurons result in failure of endogenous pain resolution pathways and drive the transition to chronic pain. Importantly, targeting mitochondrial respiration, scavenging reactive oxygen species or supplementation with nicotinamide riboside (vitamin B3) both represent potential therapeutic strategies to restore failing pain resolution pathways, thereby treating chronic inflammatory pain.”
Hanneke Willemen PhD, Center for Translational Immunology, UMC Utrecht
This research is a beacon of hope for the millions suffering from chronic pain, a condition that often leads to disability and a diminished quality of life. Current treatments for chronic pain are limited and can have severe side effects. This study opens new doors for treatment strategies, like targeting mitochondrial function or using supplements like nicotinamide riboside (a form of vitamin B3), to help our neurons recover and manage pain more effectively.
The study also sheds light on a critical aspect of pain management: the resolution of pain is not just about waiting for the pain triggers to fade away. It’s an active process involving our body’s internal pain resolution mechanisms. When these mechanisms fail, pain persists.
The research by Willemen and Eijkelkamp is a significant step forward in understanding and potentially treating chronic pain. It’s not just about managing symptoms but addressing the underlying cellular changes. For health professionals, patients, and anyone interested in the science of pain relief, this study offers new insights and hope for more effective treatments in the future.