In a development that could reshape vaccination methods, Stanford University scientists have designed a tetanus vaccine that can be delivered through the skin in the form of a cream. Published in Nature, the study uses a common skin bacteria to trigger immune responses, but the viability of such solutions is still questioned.
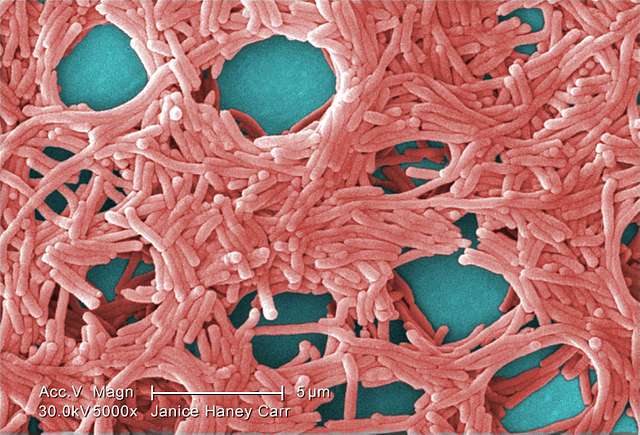
The cream contains Staphylococcus epidermidis, a bacterium commonly found on human skin. Researchers modified this bacteria to display tetanus toxin on its surface, prompting the body to produce antibodies against tetanus, which can negate the need for injective vaccines.
Wearing a Jacket with Someone Else’s Name
To start with, the researchers first identified a protein called Aap on the bacterium’s surface, which is crucial for triggering an antibody response. They modified this protein to display tetanus toxin fragments. Researchers also triggered the same response by chemically attaching the toxin to the bacteria’s surface.
“We got blood from human donors and found that their circulating levels of antibodies directed at S. epidermidis were as high as anything we get routinely vaccinated against,” said Michael Fischbach, the study’s senior author, while explaining why S. epidermidis was selected for the study.
Pre-clinical trials on mice also demonstrate some strong trends. When given lethal doses of tetanus, mice vaccinated with the cream survived, even at six times the lethal dose; however, the unvaccinated control had less life expectancy.
Similar Posts
What Is the Future of This Technology?
“We think this will work for viruses, bacteria, fungi, and one-celled parasites,” Fischbach stated. “Most vaccines have ingredients that stimulate an inflammatory response and make you feel a little sick. These bugs don’t do that.”
Fischbach further explains the importance of the discovery. “Respiratory pathogens responsible for the common cold, flu, and COVID-19 tend to get inside our bodies through our nostrils. Normal vaccines can’t prevent this. They go to work only once the pathogen gets into the blood.”
The next stage of research requires preclinical trials on primates like monkeys, with human clinical trials potentially starting after 2-3 years. These trials will address the questions about dosage and effectiveness duration of the proposed vaccines. Additionally, production costs and implementation methods require further study.
While promising, this technology faces regulatory hurdles and requires extensive safety testing. The research demonstrates potential, but implementation challenges demand careful examination before public availability.