The United States health system faces an intensifying challenge as norovirus cases surge to record levels. The Centers for Disease Control and Prevention (CDC) reports 91 outbreaks during the week of December 5, a significant increase from 69 cases in late November, and substantially higher than the previous maximum of 65 outbreaks typically observed during the same period.
Current CDC data likely understates the crisis, as over 10 states participate in the National Outbreak Reporting System, and reporting individual cases isn’t mandatory. Most healthcare facilities don’t routinely test for norovirus, and many affected individuals don’t seek medical attention, suggesting the actual case count far exceeds reported numbers.
The impact resonates across state health departments. Minnesota officials document over 40 December outbreaks, while California reported at least 80 cases linked to raw oysters at a single event. In Hawaii, authorities closed a popular hiking destination after dozens of campers contracted the virus.
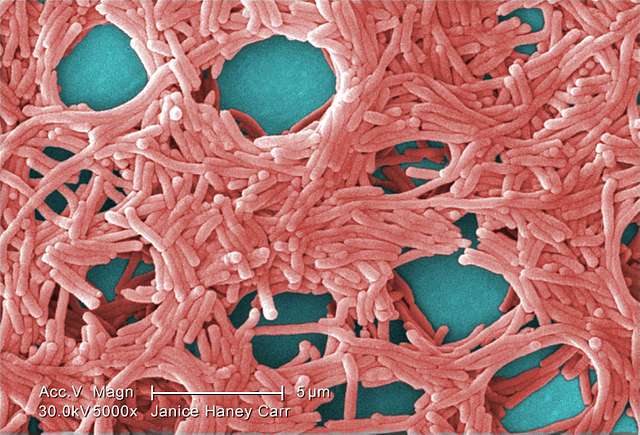
This gastroenteritis-causing virus creates a substantial public health burden. The CDC reports about 2,500 outbreaks annually, with cases occurring throughout the year but most commonly between November and April. As the leading cause of foodborne illness in the United States, norovirus remains a significant health concern.
Similar Posts
The virus presents a predictable yet challenging clinical pattern. Symptoms emerge within 12 to 47 hours post-exposure, manifesting as nausea, vomiting, stomach pain, and diarrhea. While most recover within 1-3 days, they remain contagious even after symptom resolution. The CDC identifies children under 5, older adults, and immunocompromised patients as facing elevated risks of severe infection.
Current prevention protocols require meticulous attention. The CDC emphasizes that hand sanitizer proves ineffective against norovirus, necessitating thorough hand washing with soap and water. Food safety measures demand shellfish cooking at 145°F internal temperature and careful produce washing. The virus’s extreme contagiousness—requiring only a few particles for infection—and its ability to spread through contaminated surfaces, food, and water demands enhanced vigilance.
The virus particularly impacts congregate settings including prisons, cruise ships, day care centers, and college dormitories. This winter’s elevated case numbers create significant challenges for healthcare facilities and public health departments, especially given the virus’s resistance to many common disinfection methods and its rapid person-to-person transmission in confined spaces.