A new review summarises the epidemiological evidence for the correlation between exposure to various outdoor and indoor air pollutants (mainly particulate matter (PM), nitrogen oxides (NOx), ozone (O3), and polycyclic aromatic hydrocarbons (PAHs)) and overweight and obesity outcomes in recent years. The study was executed by the researchers XiaoyiShi, YuxinZheng, Haiwen Gui, YuxiZhang, Minghui JiangFrom School of Public Health, Qingdao University,China. The study discusses the multiple effects of air pollution during exposure periods throughout life and sex differences in populations. This review also describes the potential mechanism underlying the increased risk of obesity caused by air pollution, including inflammation, oxidative stress, metabolic imbalance, intestinal flora disorders and epigenetic modifications. Finally, this review
proposes macro- and micro-measures to prevent the negative effects of air pollution exposure on the obesity prevalence.
- Obesity
According to the data reported by the Organization for Economic Co-
operation and Development (OECD) in 2019, over half of the population
in 94% of OECD member countries is overweight, and approximately
one-quarter is obese (Cecchini and Vuik, 2019). Based on BMI trends,
the obesity prevalence is reaching pandemic levels globally (Lin and Li,
2021). As stated by the WHO in 2020, 38.9 million children under 5
years are overweight globally, while 340 million adolescents and 650
million adults worldwide are obese as well (Rahayu et al., 2021). In
Korea and Japan, the incidence is less than 6%, whereas it is greater than 30% in New Zealand, Mexico, and the United States (US).
More crucially, in the last several decades, the incidence of overweight
and obesity has increased.
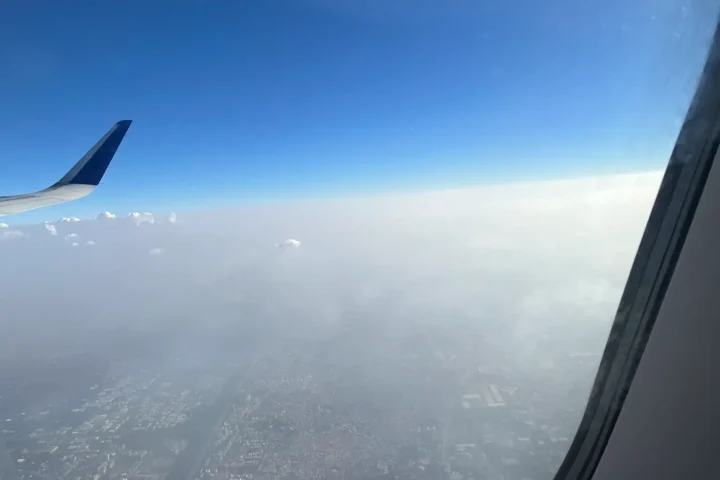
- Air pollution
An assessment has shown that air pollution contributes significantly to the increased global burden of disease cohen et-al 2007 X. Shi et al. TheLancet emphasises that air pollution is one of the main environmental factors contributing to disease and early mortality worldwide (Hahad et al., 2020), and a meta-analysis has revealed that outdoor PM2.5 exposure is related to 253 premature deaths per million population
(Waidyatillake et al., 2021). The WHO estimates that outdoor air pollution induces approximately 4.2 million annual deaths, while indoor
air pollution induces approximately 3.8 million annual deaths, mainly in
low- and middle-income countries.
4. Epidemiology
New epidemiological studies have indicated that exposure to air pollutants is closely related with obesity as well, which are listed in Table 1. Previously the studies focussed on cardiovascular and respiratory system but the new study signifies obesity & body weight.
Table 1. Epidemiological studies examining the correlation between outdoor and indoor air pollution exposure and obesity outcomes. (Body Mass Index – BMI, Particulate Matter – PM
| Study design and sample (% female) | Year and area | Exposure period | Exposure (Outdoor/indoor) | Study (population and age) | Outcome measure | Major findings | |
| Longitudinal studyN=79,992 (49) | 2011–2017Follow-up: 5 yearsSpainCatalonia | Prenatal and early life exposure | PM10, PM2.5 and NO2 (Outdoor) | ChildrenAge: birth-5 years | BMI z score | The average increase in BMI measured during follow-up per 6.3 μg/m3 increase in PM10 exposure was 0.023 kg/m2. | |
| Prospective conduct study N=1125 (47) | 2009–2014Follow-up: 5 monthsUSColorado | Prenatal exposure | PM2.5, O3 and TRAP(Outdoor) | InfantsAge: birth and 5 months | Birth weightFat massFat-free massBFP | Third trimester O3 exposure was correlated with greater adiposity at the 5-month follow-up (2.2%/IQR), and with greater rates of change in fat mass (1.8 g/day) and adiposity (2.1%/100 days) from birth to the 5-month follow-up. | |
| Longitudinal study | Enrolled1998–2006Follow-up: 5–7 yearsUSNew York | Prenatal exposure | PAHs(Outdoor and indoor) | ChildrenAge: 5 years and 7 years | BMI z scoreFat massBFP | At age 5, 21% of the children were obese, and at the age of 7 year, 25% were obese. | |
| Longitudinal study N= 535 | 1998–2006USNew York | Prenatal exposure | PAHs(Outdoor and indoor) | ChildrenAge: 5–14 years | BMI z score(Growth trajectory) | The incidence of obesity was 20.5% at age of 5%, and 33% at age of 11. In addition, the growth trajectory increased across follow-up visits until age 11. | |
| Longitudinal study N= 2318 (49.4) | 2002–2013USCalifornia | Early-life exposure | TRAP (NOx)(Outdoor) | Children age: 10 years | BMI | A 2 standard deviation difference in TRAP (NOx) exposure in the first year of life was correlated with a 0.1 kg/m2 faster increase in BMI growth annually. | |
| Cross-sectional study N=40,053 (51.7) | 2013–2014China55 county-level cities | Childhood exposure | PM2.5(Outdoor) | ChildrenAge: 6–17 years | BMI | The PM2.5-associated risk was increased in older age groups (15–18 years) (OR=4.89) and children living in urban regions (adjusted OR=1.15) (interaction p values < 0.05 | |
| Gravitational study N=2660 | 2012 Spain, Barcelona | Childhood exposure | PM2.5, EC, UFP and NO2 (Outdoor- school) PM10, PM2.5, and NO2 (Indoor- home) | Children age: 7-10 years | BMI zScore | Children exposed to the highest tertile of UFP at school had higher risk of being overweight or obese (OR=1.30) than the lowest tertile. | |
| Cross-sectional study N=1301 (45.3) | 2013-2016Europe | Childhood exposure | PM2.5 and NO2 (Outdoor and indoor) | ChildrenAge: 6–11 years | BMI z scoreWCTSTFat mass | Outdoor PM2.5 exposure was related to a higher odds of an overweight status and obesity. |
Accumulating clinical epidemiology (Barker, 2012, Shaukat et al., 2018) data and numbers confirm that pollution in early life, during the fertilised egg, embryo, infant and childhood stages, may exert an effect on long-term health and may represent the origin of adult disease through programming. This theory is called as developmental origins of health and disease (DOHaD) (Barker, 1990, Barker, 1995). DOHaD provides novel strategies for the lifelong prevention of chronic diseases (Gillman et al., 2007).
However, in a study of adults exposed to traffic pollution-related PM2.5, 53.6% of the study population was obese, but the prevalence was higher in women (55.0%) than in men (48.8%) (Zhang et al., 2020). According to the BMI, WC, WHtR and BFP, the incidence of obesity among women was higher than that among men in the Chinese rural cohort study mentioned above. The obesity rates based on BMI, WC, WHtR, and BFP among women were 64.63%, 73.2%, 64.16% and 72.12%, respectively. In contrast, the corresponding percentages among men were 35.37%, 26.8%, 35.84% and 27.88%, respectively, which were lower than those among women (Liu et al., 2020).
Prevention
- The ultimate goal of exploring the relationship and causes of air pollution and obesity is the precise prevention and control of obesity.
- Individual protection should not be ignored. People can wear masks outdoors and use air purifiers indoors to reduce the intake of air pollutants. Based on a systematic review, the use of air purifiers can reduce indoor PM2.5 levels by 11.45 μg/m3.
- Exposure monitoring is also essential. Medical institutions detect internal exposure doses of air pollution using convenient and advanced methods to assess people at risk in a timely manner
- Attention to diet might also play a protective role in reducing the effects of air pollution and preventing obesity
Conclusion
There is clear and considerable evidence of a link between air pollution, particularly PM and the risk of overweight/obesity during different life stages. Multilevel public health and policy interventions are needed to address this worldwide burden for obesity prevention. Specific and in-depth studies on air pollution and the risk of obesity are more limited. Further research on specific components of PM, sensitive exposure period, threshold dose range is needed along with research on the effectiveness of precise interventions and measures for obesity prevention.