Melbourne is grappling with a serious measles outbreak that health officials warn shows no signs of slowing down. Victoria has recorded over 20 cases so far in 2025, already surpassing the entire total for 2024, marking the state’s worst outbreak in over ten years.
What’s particularly concerning is that the virus is now spreading locally. While previous outbreaks typically involved travelers bringing measles into Australia, Victoria’s Chief Health Officer Dr. Tarun Weeramanthri confirmed that “a growing number of measles cases have acquired their infection locally in Victoria.”
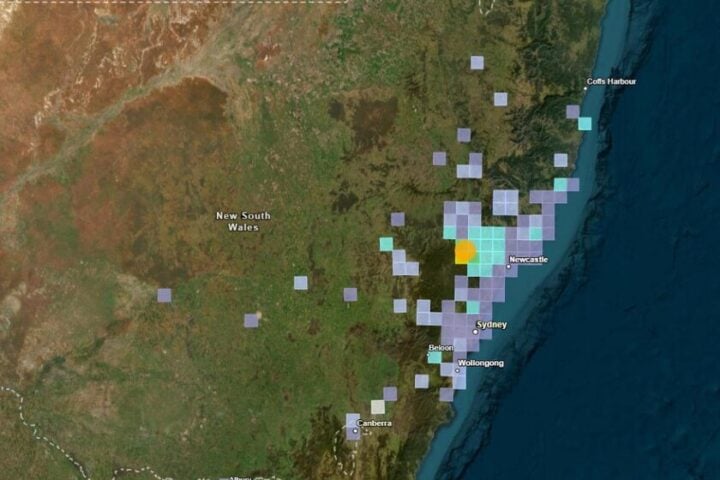
The outbreak has forced health authorities to issue warnings about multiple exposure sites across greater Melbourne and Mitchell Shire. These include Melbourne International Airport, Westfield Fountain Gate shopping center, and several locations in Kilmore including the local Coles, ALDI, library, and district hospital.
A recent case involved a traveler who returned from Pakistan and was infectious on Emirates flight EK 408 arriving in Melbourne on April 24. Another case was linked to a Vietnam Airlines flight from Ho Chi Minh City that landed on April 20.
“There is currently an increased risk of measles in greater Melbourne and Mitchell Shire, in addition to the ongoing risk of measles importation in Victoria,” Dr. Weeramanthri said.
The surge in local cases mirrors a worrying global trend. Countries across Southern and Southeast Asia, Eastern Europe, and the United States are experiencing their own outbreaks with cases nearly thousands.
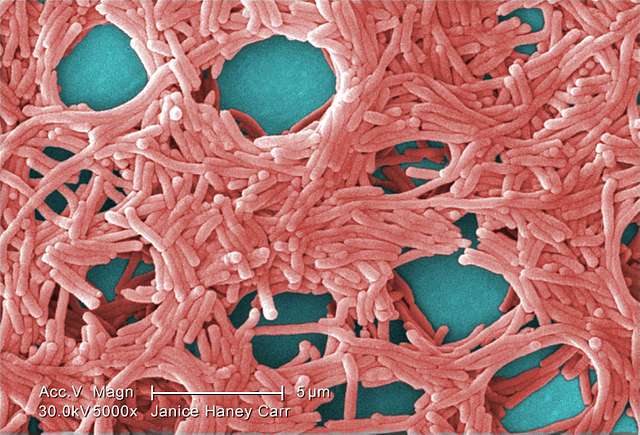
Measles spreads remarkably easily. The virus can linger in the air or on surfaces for up to two hours after an infected person has left the area. People are contagious from 24 hours before symptoms appear until four days after the rash develops.
Symptoms typically show up 7 to 18 days after exposure and include fever, cough, red eyes, runny nose, and feeling generally unwell. A distinctive red rash then develops, usually starting on the face before spreading downward.
Similar Posts
“Measles is a highly infectious disease that can lead to uncommon but serious complications, such as pneumonia and brain inflammation,” Dr. Weeramanthri warned.
Several groups face higher risks from measles. These include infants under 12 months who are too young to have received both vaccine doses, pregnant women, people with weakened immune systems, and anyone not fully vaccinated.
Victorian vaccination rates have dropped below the national target of 95% since the COVID-19 pandemic. Health officials note that “the majority of recent cases have arisen in people who have not had two documented doses of the MMR vaccine.”
The MMR (measles-mumps-rubella) vaccine remains the most effective protection against the virus. It requires two doses for full immunity. The vaccine is free for all Victorians and available at GPs, pharmacies, local councils, and Aboriginal Health Services. No Medicare card is required to receive the state-funded vaccine.
Health authorities are urging anyone born during or after 1966 who hasn’t had two documented doses, or is unsure of their vaccination status, to get vaccinated immediately.

Anyone who visited the listed exposure sites should monitor for symptoms for up to 18 days after exposure. If symptoms develop, medical attention should be sought promptly. People are advised to call ahead to the healthcare provider and wear a mask to prevent potentially exposing others.
With measles outbreaks reported in multiple countries including Pakistan, Indonesia, Vietnam, Thailand, India, parts of Africa, Europe, the UK, the Middle East, and North America, officials strongly recommend that anyone planning overseas travel ensure their vaccinations are up to date.
The current situation serves as a stark reminder that even diseases we once thought were largely under control can quickly resurge when vaccination rates decline.