A fascinating breakthrough has emerged from the depths of the microbiome – the trillions of microscopic organisms inhabiting our digestive tracts. It turns out that the high-fat, low-carbohydrate ketogenic diet, often seen as a trendy weight-loss method, possesses hidden powers beyond shedding pounds. This diet has been an unexpected hero in the battle against seizures, especially for children with epilepsy who don’t respond to conventional medications.
A recent study led by Gregory Lum, a postdoctoral researcher at UCLA, has unveiled a remarkable connection between the ketogenic diet, the gut microbiome, and seizure protection in mice. This discovery sheds light on the potential development of new therapies that harness the benefits of this diet while bypassing its strict requirements and unpleasant side effects. Let’s dive into the intriguing world of the gut-brain connection and its implications for pediatric epilepsy patients.
The ketogenic diet, known as KD, is already renowned as a potent treatment for refractory epilepsy, especially in children resistant to anti-seizure medications. It boasts an impressive track record, with approximately 30% of children on KD becoming seizure-free and about 60% experiencing a significant reduction in seizure frequency. However, KD’s effectiveness is often hindered by challenges related to dietary compliance, side effects such as nausea, constipation, and fatigue, and the reluctance of patients to adopt such a drastic dietary change.
What sets this study apart is its focus on the gut microbiome’s role in mediating the effects of the ketogenic diet on metabolism, neural activity, and behavior. Previous research had hinted at the diet’s impact on the gut microbiome, but specifics varied between studies. To unravel the gut-brain connection, Lum and his team decided to explore how the diet’s changes in the human gut microbiome could be transferred to mice and, in turn, protect them against seizures.
Lum collected fecal samples from 10 pediatric epilepsy patients who had not responded to traditional anti-seizure medications but had undergone ketogenic diet therapy. These samples were taken both before and after one month on the diet. What Lum discovered was nothing short of astonishing.
Mice that received fecal transplants from patients who had been on the ketogenic diet for a month displayed increased resistance to seizures compared to those who received pre-diet fecal transplants. This finding is groundbreaking, highlighting the gut microbiome as a key player in the fight against seizures.
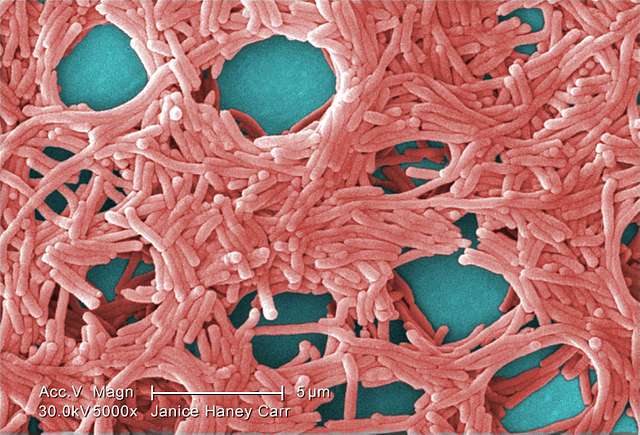
Furthermore, the study revealed that the ketogenic diet induced critical changes in gut microbiome functions related to fatty acid oxidation and amino acid metabolism, and these changes were maintained when the fecal matter was transferred to the mice. In other words, the diet reshaped the gut microbiome in ways that were beneficial for seizure protection.
While more research is needed to fully comprehend these changes, Lum’s study offers hope for developing microbiome-based therapies for pediatric epilepsy patients who don’t respond to standard anti-seizure medications. Lum himself commented, “Narrowing down the functions of the microbes that are beneficial toward seizure protection can potentially lead to new ways to enhance the efficacy of the ketogenic diet or to mimic its beneficial effects.”
Similar Posts
The study also delved into the intricate details of the gut microbiome, employing metagenomic sequencing to reveal shared functional features in post-KD fecal microbiota across the patients. Notably, alterations in metabolic pathways related to methionine, glycine, serine, and betaine metabolism were observed, suggesting a microbiome-dependent role in the diet’s efficacy.
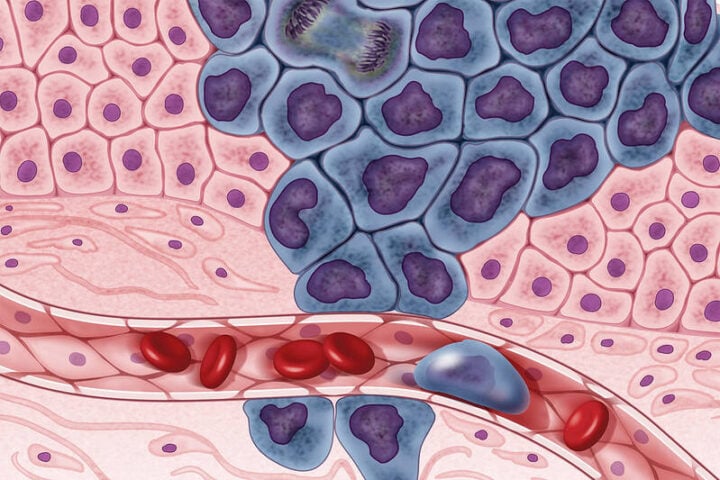
Remarkably, when the microbiota from KD-treated pediatric epilepsy patients was introduced into mice, the rodents displayed increased resistance to seizures. Transcriptomic profiling of brain tissues from these mice revealed differentially expressed genes linked to core cell biological processes, further emphasizing the microbiome’s influence on seizure protection.
This study provides compelling evidence that the ketogenic diet, by altering the gut microbiome, can contribute significantly to shielding against seizures. The connections between microbial genomic pathways, metabolites, and hippocampal transcripts related to epilepsy suggest a complex interplay between these elements. Additionally, the enrichment of hippocampal differentially expressed genes in epilepsy genome-wide association studies implies a potential link to genetic risk for human epilepsy.
This research opens up a new frontier in the treatment of refractory epilepsy, offering hope to those who have struggled to find relief through conventional means. The gut-brain connection, once a mystery, now holds the promise of unlocking more effective therapies, potentially transforming the lives of children with epilepsy. While the journey to harnessing these discoveries for practical applications is ongoing, the path ahead is illuminated by the fascinating world of the gut microbiome and its role in our health and well-being.