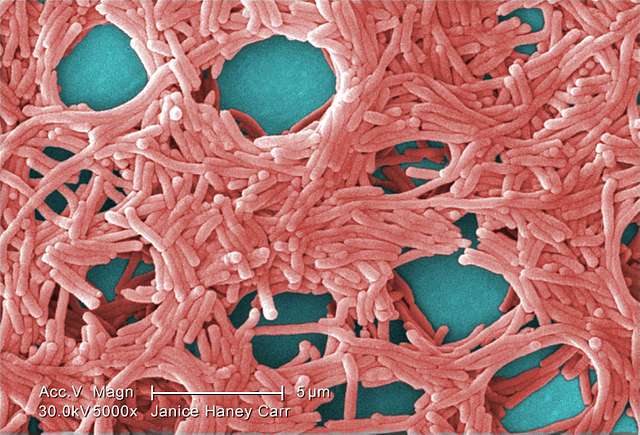
With an emphasis on RNA interference, a ground-breaking Northwestern Medicine study that was just published in Nature Communications offers a fresh perspective on neuronal death in Alzheimer’s disease. The important role that short RNA strands play in the development of Alzheimer’s and possibly other neurodegenerative diseases is revealed by this important study. Marcus Peter, the Tom D. Spies Professor of Cancer Metabolism at Northwestern University Feinberg School of Medicine, and his team, carried out the study, led by first author Bidur Paudel.
Millions of people suffer from Alzheimer’s disease, which is characterized by a sharp deterioration in cognitive function due to brain cell death. The identification of toxic short RNAs (sRNAs), which contribute to DNA damage and brain cell death in old and Alzheimer’s brains, is a key finding of this work. When protective sRNAs decline with age, more harmful sRNAs that are often controlled by them proliferate. It is suggested that a major contributing element to the onset of Alzheimer’s is this imbalance. The discovery that microRNAs are the main protective sRNAs, serving as gatekeepers to stop harmful sRNAs from entering the cellular machinery that causes RNA interference, is the key finding.
The study also sheds light on a fascinating subset of people called SuperAgers—those over 80 who have memory capacities comparable to those of people in their 20s and 30s. Higher concentrations of protective short RNA strands in these people’s brain cells may be related to their better memory retention.
This discovery provides a fresh direction in terms of therapy implications. With varying degrees of effectiveness, traditional Alzheimer’s treatments have mostly targeted the reduction of amyloid plaques or the prevention of tau phosphorylation. The results of this study point to a potential new treatment strategy for Alzheimer’s and other neurodegenerative diseases: either stabilizing or producing more of these beneficial short RNAs. Even if there are medications like these, more research and development in animal models are required.
“The overwhelming investment in Alzheimer’s drug discovery has been focused on two mechanisms: reducing amyloid plaque load in the brain — which is the hallmark of Alzheimer’s diagnosis and 70 to 80 percent of the effort — and preventing tau phosphorylation or tangles. However, treatments aimed at reducing amyloid plaques have not yet resulted in an effective treatment that is well tolerated. Our data support the idea that stabilizing or increasing the amount of protective short RNAs in the brain could be an entirely new approach to halt or delay Alzheimer’s or neurodegeneration in general.”
– Marcus Peter, PhD, Tom D. Spies Professor of Cancer Metabolism and a professor of Medicine in the Division of Hematology and Oncology.
The study’s methodology included examining the brains of young and old mice modelled for Alzheimer’s disease, neurons derived from induced pluripotent stem cells from patients with and without the disease, and numerous human brain-derived neuron-like cell lines that were exposed to amyloid beta fragments. This thorough method has made a major contribution to our understanding of how sRNAs function in Alzheimer’s disease.
These discoveries have broad ramifications since they imply that the ratio of protective to harmful sRNAs plays a crucial role in the development of neurodegenerative illnesses. The research offers a fresh viewpoint on the molecular mechanisms behind these illnesses and creates new avenues for potential treatment approaches.