Pertussis, commonly known as whooping cough, causes a distinctive gasping sound when infants struggle to breathe during coughing attacks. This bacterial infection is resurging across the United States in 2025, with significant implications for public health.
“Whooping cough is most severe in young children, and particularly infants under one year of age, especially those who haven’t received their initial vaccinations for whooping cough or pertussis,” Dr. Nicolas Cortes-Penfield of the University of Nebraska Medical Center explains. “However, it can also cause severe disease in adults who have underlying immune problems. So for example, let’s say you’re receiving chemotherapy for cancer or you’ve had an organ transplant or if you have some sort of underlying lung disease.”
Current Outbreak Data
CDC data confirms 8,077 U.S. pertussis cases reported in early 2025—more than double the 3,847 cases from the same period last year. This surge follows a predictable pattern after the pandemic lull, and 2025 could potentially see the highest number of cases since 1948.
The CDC states that “reported cases of whooping cough (pertussis) continue to be elevated nationwide.” Alameda County Health also reports that “pertussis (whooping cough) is on the rise in California and nationwide.”
For perspective, before vaccines became available in the 1940s, more than 200,000 cases occurred annually in the U.S.
How Whooping Cough Spreads
The CDC emphasizes that whooping cough is very contagious and can spread easily from person to person. This high transmissibility makes community vaccination especially important.
When an infected person coughs or sneezes, tiny droplets containing the bacteria spread through the air. The disease is most contagious during the early stages when symptoms resemble a common cold.
Who’s Most at Risk?
“Babies younger than 1 year old are at highest risk of severe disease and complications,” the CDC states. Approximately one-third of infants under one year who contract pertussis require hospitalization, with a 1% mortality rate among complicated cases.
Adults with compromised immune systems or underlying lung conditions like COPD or cystic fibrosis also face higher risks.
The Vaccine Schedule: Your Best Defense
Philadelphia Public Health’s guidance is clear: “Your baby needs 4 doses of the DTaP vaccine to keep them safe from diphtheria, tetanus, and whooping cough. Talk to their doctor or call a city health center to get them vaccinated.”
The full CDC-recommended schedule includes:
- Five DTaP doses at ages 2, 4, 6, 15-18 months, and 4-6 years
- A Tdap booster at 11-12 years
- Tdap during each pregnancy (ideally between 27-36 weeks)
- Adult boosters every 10 years
Protecting Pregnant Women and Newborns
Alameda County Health advises: “Protect yourself and your baby—get the Tdap vaccine during the third trimester. Talk to your provider & learn more.”
This timing maximizes antibody transfer to the baby before birth, providing critical protection during their first vulnerable months of life before they can receive their own vaccinations.
Similar Posts
“CDC recommends that pregnant women get Tdap during the 27th through 36th week of each pregnancy, preferably during the earlier part of this time period.” the CDC urges pregnant women.
The Cocooning Strategy
Protection extends beyond vaccinating just children. The “cocooning” approach—ensuring all household members and caregivers are fully vaccinated—creates a protective bubble around vulnerable infants too young for immunization.
This strategy becomes even more critical as exemption rates climb—kindergarten vaccine exemptions rose to 3.3% in 2023-24, with 14 states exceeding 5%.
Symptoms to Watch For
Early pertussis typically resembles a common cold with:
- Runny nose
- Mild cough
- Low-grade fever (often mild or absent)
- Sneezing
After 1-2 weeks, symptoms often progress to:
- Severe coughing fits
- The characteristic “whoop” sound when gasping for air after coughing
- Vomiting after coughing episodes
- Exhaustion
- In infants: breathing difficulties, apnea, or cyanosis (turning blue) rather than the classic “whoop”
The Economic Impact
Pertussis imposes significant costs on families and healthcare systems. Studies show considerable variation in cost estimates: CDC reports approximate $2,172 per case in school outbreaks, other analyses estimate $315-$2,269 per case, with costs including medical care, lost work time, and caregiver burden.
Treatment and Post-Exposure Guidelines
For treatment, macrolides such as azithromycin are preferred for individuals aged one month and older. For infants under one month, azithromycin is specifically recommended due to the risk of infantile hypertrophic pyloric stenosis associated with erythromycin.
If exposed to pertussis:
- Close contacts should receive antibiotic prophylaxis (typically azithromycin) within 21 days of exposure
- Infected individuals must stay home until 5 days after starting antibiotics
- Untreated cases should remain isolated for 21 days after cough onset

What You Can Do
The CDC states: “The best way to prevent complications from whooping cough is to get vaccinated.”
- Check vaccination records for everyone in your household
- Talk to your healthcare provider about boosters if it’s been more than 10 years
- Ensure pregnant women receive Tdap during the third trimester
- Watch for persistent coughing fits, especially those followed by vomiting or gasping
- Seek medical attention promptly if symptoms develop
- Practice good hygiene and stay home when sick
As cases continue to rise nationwide, vaccination remains our most effective tool for protecting vulnerable populations—especially infants too young to be fully immunized.
FAQWhat exactly is whooping cough and why is it called that?
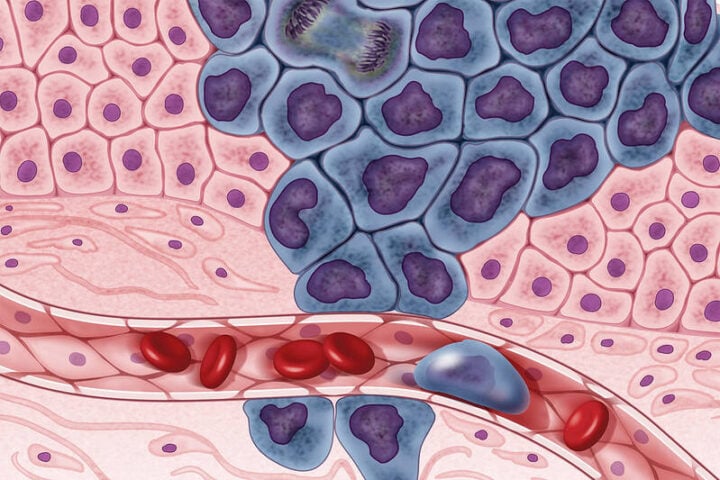
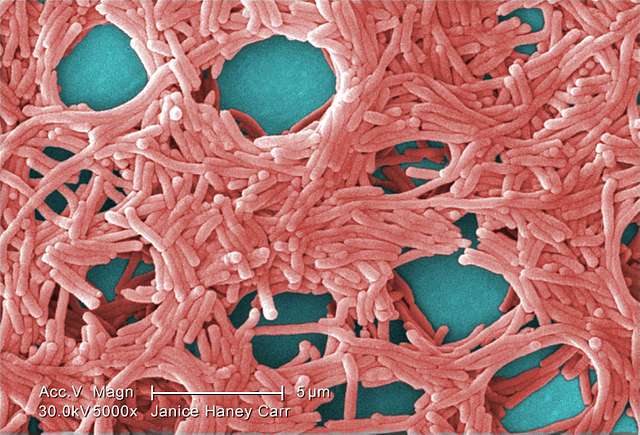
Whooping cough (medically known as pertussis) is a highly contagious bacterial infection that affects the lungs and breathing tubes. It gets its name from the distinctive “whoop” sound many people make when gasping for air after a severe coughing fit. The disease is caused by bacteria called Bordetella pertussis, which attach to the tiny hair-like structures in the lungs, causing inflammation and swelling.
How many cases of whooping cough are there right now?
According to CDC data, there are 8,077 confirmed cases of whooping cough in the United States so far in 2025. This is more than double the 3,847 cases reported during the same period last year. Health officials are concerned about this rapid increase, which follows a pattern of lower transmission during the COVID-19 pandemic years.
Who is most at risk from whooping cough?
Babies under 1 year old face the highest risk of severe complications and death from whooping cough. About one-third of infants who catch pertussis require hospitalization, and there’s a 1% mortality rate among complicated cases. Adults with weakened immune systems (like those on chemotherapy or who’ve had organ transplants) and people with underlying lung conditions (such as COPD or cystic fibrosis) are also at higher risk of severe disease.
What does whooping cough look like in babies?
In babies, whooping cough often doesn’t cause the classic “whoop” sound. Instead, infants might:
- Have brief periods where they stop breathing (apnea)
- Turn blue or purple (cyanosis) from lack of oxygen
- Struggle to breathe, feed, or drink
- Have coughing fits followed by vomiting
- Show extreme fatigue
- Have seizures (in severe cases)
These symptoms can be life-threatening and require immediate medical attention.
How can I tell if my child has a cold or whooping cough?
Early whooping cough can look like a common cold with symptoms like runny nose, mild cough, and low-grade fever. The difference becomes clear after 1-2 weeks when whooping cough progresses to severe coughing fits that:
- Come in rapid bursts where the person can’t catch their breath
- Often end with a “whooping” sound when breathing in (though not always in babies)
- Frequently cause vomiting afterward
- Leave the person extremely tired
- Get worse at night
- Continue for weeks or even months (sometimes called the “100-day cough”)
If your child has been coughing for more than a week or has coughing fits that match these descriptions, contact your healthcare provider right away.
What vaccines do my family need to prevent whooping cough?
The CDC recommends these vaccinations to protect against whooping cough:
- Babies and children: Five doses of DTaP vaccine at 2 months, 4 months, 6 months, 15-18 months, and 4-6 years
- Preteens: One Tdap booster shot at 11-12 years
- Pregnant women: Tdap vaccine during the third trimester (ideally between 27-36 weeks) of EACH pregnancy
- Adults: One Tdap shot if you haven’t had one before, then a Td or Tdap booster every 10 years
- Caregivers and family members: Everyone who will be around newborns should be up-to-date on their whooping cough vaccines (this is called “cocooning”)
If someone in my child’s school has whooping cough, what should I do?
If there’s a whooping cough case at your child’s school:
- Check that your child is up-to-date on vaccinations
- Watch for symptoms like persistent cough, especially one that gets worse at night
- Contact your doctor if your child develops a persistent cough or has been in close contact with someone diagnosed with pertussis
- Follow school guidelines about possible exclusion periods
- If your child is prescribed antibiotics for whooping cough exposure, make sure they complete the full course
- Know that your child should stay home until they’ve completed 5 days of antibiotics if diagnosed
How is whooping cough treated?
Whooping cough is treated with antibiotics, typically macrolides like azithromycin. Important treatment facts:
- Antibiotics work best when started early, ideally during the first 1-2 weeks of symptoms
- Even with antibiotics, the cough may last for weeks or months
- People with whooping cough should stay home until they’ve completed 5 days of antibiotics
- Close contacts (household members, caregivers) may need preventive antibiotics even if they don’t have symptoms
- For infants and severe cases, hospitalization may be necessary for oxygen support, monitoring, and assistance with breathing
Why are whooping cough cases increasing despite vaccinations?
Whooping cough cases are rising for several reasons:
- Protection from vaccines wanes over time, creating immunity gaps even in vaccinated people
- Kindergarten vaccine exemption rates have increased to 3.3% nationally, with 14 states exceeding 5%
- The bacteria that cause whooping cough have evolved slightly, making vaccines somewhat less effective than in the past
- After the COVID-19 pandemic’s social distancing and masking reduced spread, we’re now returning to more normal interaction patterns
- Better testing and reporting methods may be catching more cases that would have been missed previously
Despite these challenges, vaccination remains the most effective way to prevent severe disease and complications.

![Big city Los Angeles smog building [photo source: pixabay] [PDM 1.0]](https://www.karmactive.com/wp-content/uploads/2025/04/46-of-Americans—156-M—Now-Breathe-Hazardous-Smog-and-Soot-State-of-the-Air-Report-Exposes-Decade-High-Pollution-1.jpg)