Grace Davidson has made UK medical history by becoming the first woman in the country to give birth after receiving a womb transplant. Her daughter, Amy Isabel, was born on February 27, 2025, at Queen Charlotte’s and Chelsea Hospital in London, weighing 4 pounds, 8 ounces (2.04kg).
This landmark birth marks a significant breakthrough for women with absolute uterine factor infertility (AUFI), a condition affecting approximately one in 5,000 women in the UK. These women either are born without a uterus or have had it removed.
“It was quite overwhelming because we’d never really let ourselves imagine what it would be like for her to be here,” said Grace, describing the moment she first held her daughter. “It was really wonderful.”
A Sister’s Extraordinary Gift
Grace, a 36-year-old NHS dietitian from north London, was born with Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome, which meant she did not have a functioning womb. Her 42-year-old sister, Amy Purdie, who already had two children of her own aged 10 and 6, donated her womb in February 2023.
“It was incredibly difficult to let her do that for me,” Grace said. “It’s a huge act of sisterly love.”
The transplant surgery took place at the Churchill Hospital in Oxford following years of planning and preparation. A team of more than 30 medical professionals worked for approximately 17 hours to complete the procedure.
Amy Purdie described watching her sister become a mother as “an absolute joy” and “worth every moment” of what she went through to donate her womb. Remarkably, Grace had her first-ever period within two weeks of the transplant and became pregnant on her first attempt at IVF.

A Long-Awaited Journey
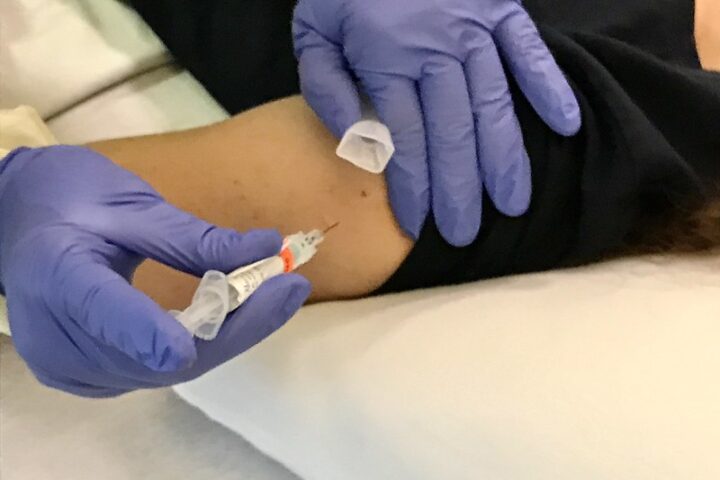
The path to parenthood was not quick or simple for Grace and her husband Angus, 37. Before receiving the donated womb, the couple underwent fertility treatment to create and freeze seven embryos through IVF.
“We’d been intending to have a family somehow since we were married, and we’ve kind of been on this journey for such a long time,” Angus explained. “The moment we saw her was incredible, and both of us just broke down in emotional tears.”
The couple named their daughter Amy Isabel – after Grace’s sister who donated the womb, and Isabel Quiroga, the surgeon who helped perfect the transplant technique.
Isabel Quiroga, who led the transplant team at the Churchill Hospital in Oxford, described the procedure as “life-enhancing and life-creating.” She noted that while the procedure carried risks for both sisters, the benefits were extraordinary.
Similar Posts:
The Future of Womb Transplantation
This successful birth follows more than 25 years of pioneering research led by Professor Richard Smith, clinical lead at Womb Transplant UK and consultant gynaecological surgeon at Imperial College Healthcare NHS Trust.
“I’m not often short of words but when the baby came out I was speechless – there were a lot of tears in the theatre that day,” said Professor Smith. “The whole thing is astonishing and incredibly moving.”
Since Grace’s procedure, three more womb transplants have been performed in the UK using deceased donors. The medical team has permission to perform a total of 15 womb transplants as part of a clinical trial – five with living donors and ten with deceased donors.
Globally, around 135 womb transplants have been carried out in more than a dozen countries since the first successful birth in Sweden in 2014. Approximately 65 babies have been born worldwide through this procedure.
Each transplant costs around £30,000. Currently, the procedures are funded by Womb Transplant UK, with medical staff donating their time for free. The charity has sufficient funds to support two more transplants.

Medical Considerations and Next Steps
Grace takes daily immunosuppressant medication to prevent her body from rejecting her sister’s womb. These drugs can increase the risk of developing certain cancers if taken long-term.
The couple hopes to have a second child using the transplanted womb. After that, the donated womb will be removed, allowing Grace to stop taking immunosuppressants. Surgeon Isabel Quiroga notes that once the womb is removed, the associated health risks should return to baseline levels.

This breakthrough offers new hope to approximately 15,000 women of childbearing age in the UK who do not have a functioning uterus, including around 5,000 who were born without a womb.
Professor Smith emphasized that the birth of Amy Isabel will give these women hope. Around ten women already have embryos in storage or are undergoing fertility treatment – a requirement for being considered for womb transplantation.
For Grace and Angus Davidson, the journey has transformed their lives. “It sort of feels like there’s a completeness now where there maybe wasn’t before,” Grace reflected, cradling her miracle daughter – the product of medical innovation and a sister’s extraordinary love.
Frequently Asked Questions
Mayer-Rokitansky-Küster-Hauser (MRKH) syndrome is a rare condition where women are born with an underdeveloped or absent uterus, affecting about 1 in 5,000 women. While women with MRKH have functioning ovaries and produce eggs, they cannot carry a pregnancy naturally without interventions like womb transplantation. This condition is typically diagnosed during adolescence when menstruation fails to begin.
A womb transplant involves surgically transferring a uterus from a donor (living or deceased) to a recipient. Candidates typically include women with absolute uterine factor infertility (AUFI) who have viable ovaries. Before being considered, recipients must undergo fertility treatment to create and freeze embryos. The procedure requires a team of specialized surgeons and takes many hours to complete. Recipients must take immunosuppressant medication to prevent organ rejection throughout the pregnancy.
Womb transplants carry significant risks for both donors and recipients. For living donors, there are surgical risks similar to those of a hysterectomy. Recipients face risks of surgery, organ rejection, and complications from long-term immunosuppressant medications, which can increase cancer risks and susceptibility to infections. Pregnancies in transplanted wombs are considered high-risk and typically require delivery by planned cesarean section before full term.
No, womb transplants are generally temporary. After completing their desired number of pregnancies (typically one or two), recipients undergo surgery to remove the transplanted uterus. This is done to allow them to stop taking immunosuppressant medications, which carry long-term health risks. Once removed, health risks associated with these medications should return to normal baseline levels.
As of early 2025, approximately 65 babies have been born through womb transplants worldwide. The first successful birth occurred in Sweden in 2014, and since then about 135 womb transplants have been performed across more than a dozen countries including the US, China, France, Germany, India, and Turkey. The UK’s first womb transplant birth in February 2025 represents a significant milestone in this developing medical field.
In the UK, each womb transplant costs around £30,000. Currently, these procedures are funded by the charity Womb Transplant UK, with medical staff donating their time for free. The charity has indicated it has sufficient funds for only two more transplants. In most countries, womb transplants are still considered experimental and are not typically covered by standard health insurance. Whether the NHS might fund these procedures in the future remains an open question.